J Orthop Sports Phys Ther. .
Abstract
Study design: Systematic review and meta-analysis.
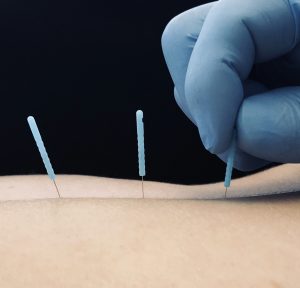
Background: Myofascial pain syndrome (MPS) is associated with hyperalgesic zones in muscle called myofascial trigger points. When palpated, active myofascial trigger points cause local or referred symptoms, including pain. Dry needling involves inserting an acupuncture-like needle into a myofascial trigger point, with the goal of reducing pain and restoring range of motion.
Objective: To explore the evidence regarding the effectiveness of dry needling to reduce pain in patients with MPS of the upper quarter.
Methods: An electronic literature search was performed using the key word dry needling. Articles identified with the search were screened for the following inclusion criteria: human subjects, randomized controlled trial (RCT), dry needling intervention group, and MPS involving the upper quarter. The RCTs that met these criteria were assessed and scored for internal validity using the MacDermid Quality Checklist. Four separate meta-analyses were performed: (1) dry needling compared to sham or control immediately after treatment, (2) dry needling compared to sham or control at 4 weeks, (3) dry needling compared to other treatments immediately after treatment, and (4) dry needling compared to other treatments at 4 weeks.
Results: The initial search yielded 246 articles. Twelve RCTs were ultimately selected. The methodological quality scores ranged from 23 to 40 points, with a mean of 34 points (scale range, 0-48; best possible score, 48). The findings of 3 studies that compared dry needling to sham or placebo treatment provided evidence that dry needling can immediately decrease pain in patients with upper-quarter MPS, with an overall effect favoring dry needling. The findings of 2 studies that compared dry needling to sham or placebo treatment provided evidence that dry needling can decrease pain after 4 weeks in patients with upper-quarter MPS, although a wide confidence interval for the overall effect limits the impact of the effect. Findings of studies that compared dry needling to other treatments were highly heterogeneous, most likely due to variance in the comparison treatments. There was evidence from 2 studies that lidocaine injection may be more effective in reducing pain than dry needling at 4 weeks.
Conclusion: Based on the best current available evidence (grade A), we recommend dry needling, compared to sham or placebo, for decreasing pain immediately after treatment and at 4 weeks in patients with upper-quarter MPS. Due to the small number of high-quality RCTs published to date, additional well-designed studies are needed to support this recommendation.
 Blog de Fisioterapia Fisioterapia
Blog de Fisioterapia Fisioterapia



